In a recent article published by Yale Climate Connections, Charles Leonard, PharmD, MSCE, FISPE—Associate Professor of Epidemiology in the Department of Biostatistics, Epidemiology and Informatics (DBEI) in the Perelman School of Medicine—highlighted how rising temperatures can impact individuals with type 2 diabetes.
A 2022 study co-authored by Leonard and other DBEI and Center for Real-World Effectiveness and Safety of Therapeutics (CREST) researchers, including Kacie Bogar, MS; Colleen M. Brensinger, MS; Sean Hennessy, PharmD, PhD; James H. Flory, MD, MSCE; and Warren B. Bilker, PhD, found that extreme outdoor temperatures increased the risk of some life-threatening conditions for people with type 2 diabetes, such as hypoglycemia and ventricular arrhythmia, a condition in which the heart beats erratically or at a slower or faster pace, which can lead to fainting or cardiac arrest.
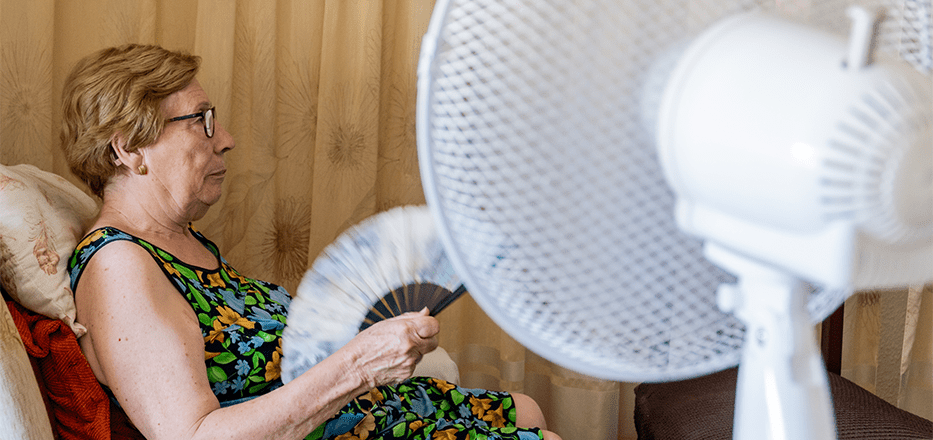
According to Leonard, these individuals “can experience a blunted response to extreme ambient heat, driven by reduced skin blood flow and an impaired sweating response, such that one’s body cannot cool itself properly.” This makes heat exhaustion more likely, and the problem “can be exacerbated by some prescription medications that further impair sweating.”
Leonard also shared that extreme heat can also increase the risk of swings in blood sugar levels, causing confusion, loss of coordination, blurry vision, slurred speech, or even seizures. Heat can also make it more complicated for clinicians to know how much medicine to prescribe due to possible side effects associated with extreme temperatures.
The World Health Organization reports diabetes has skyrocketed by 315% since 1990, especially in low to middle income countries. A 2017 study suggests that rising global temperatures may explain some of that increase, perhaps by reducing the activity of a certain kind of fat. The researchers found that a one-degree Celsius rise in temperature could cause over 100,000 new diabetes cases annually in the U.S. alone.
Leonard stressed the importance of patients with type 2 diabetes discussing strategies to manage extreme heat with their doctors. “While some preparedness examples might include identifying and seeking climate-controlled spaces, especially during the hottest part of the day, avoiding certain outdoor physical activities, staying hydrated, and checking one’s blood sugar more frequently, advice from one’s own medical provider should guide specific actions.”