While many studies have looked at how to limit patients to a short course of opioids, few have examined the other side of the issue: Are there some patients for whom longer-term use might be necessary, effective and safe? In a recent study, researchers used individual patient-level safety studies to look at people who were treated with abuse-deterrent formulations of oxycodone and hydrocodone for up to 12 months to address their chronic non-cancer pain.
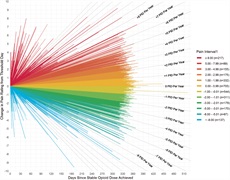
The patients met specific criteria for maintaining long-term benefit: They experienced stable or less pain, took a stable or lower opioid dose, and—in a subgroup where it could be measured—showed stable or better physical function. The findings confirm that some patients—about 44 percent of the 3192 in the first analysis, and 34 percent of the 985 in the second—do maintain pain relief. In situations where non-steroidal anti-inflammatory drugs (NSAIDs) are contraindicated, or they or other non-opioid approaches do not provide adequate pain relief, the researchers say that a trial of opioids may be considered for an appropriately selected population of chronic pain patients, with careful monitoring over time. “The criteria for such a regimen are complex,” comments lead author John Farrar, MD, PhD, and while clinicians should consider it for a carefully selected group of patients, the regimen will not be appropriate for all. But as the US population ages, the authors write, we should consider all possible therapies to relieve pain that interferes with quality of life.
The team notes that this observational study did not examine what might have happened to the same patients had they never started opioids. Future studies, they say, should more thoroughly assess a broader range of patients and the rescue medication they received, and could be designed to randomly withdraw patients from treatment in a blinded fashion multiple times over the course of 12 months, in order to demonstrate ongoing efficacy.
Authors:
John T Farrar, Warren B Bilker, Philip T Cochetti, Charles E Argoff, Jennifer Haythornthwaite, Nathaniel P Katz, Ian Gilron